Ever wondered why your gums bleed or hurt sometimes?
Quick Facts
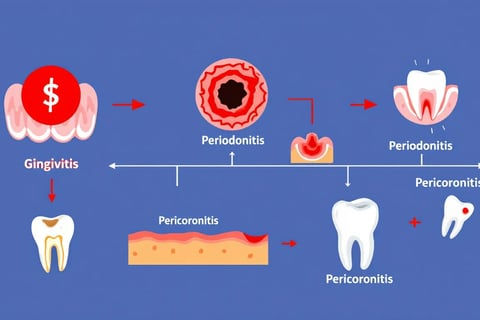
Gingivitis is the earliest stage of gum disease and is reversible with good oral hygiene and regular cleanings.
Chronic periodontitis will lead to tooth loss if left untreated, so get regular check ups and act early.
Aggressive periodontitis can cause rapid tissue damage and requires early diagnosis and treatment so monitor symptoms closely.
Gingivitis: The First Stage
Gingivitis is the earliest and mildest stage of gum disease and is reversible if treated on time. The condition is caused by the accumulation of dental plaque and leads to inflammation of the gums which then become red, swollen and bleed during brushing or flossing.
Despite showing scary signs like sensitivity and bleeding, gingivitis can be managed with good oral hygiene and regular professional cleanings. For more severe cases, scaling and root planing is done to clean below the gum line where a regular toothbrush can’t reach. This removes the tartar and plaque that’s causing irritation to the gingival tissues.
Good oral hygiene by brushing daily, flossing regularly and getting regular check ups at the dentist’s office is key to stopping periodontal diseases from progressing. By treating gingivitis early you can reverse its effects and have healthy gums again.
Chronic Periodontitis: Slow Progression
Periodontal disease also known as gum disease starts with chronic periodontitis. This condition is characterized by the gradual breakdown of tissue and bone around the teeth due to bacterial accumulation in plaque at the gum line. This leads to symptoms like bad breath, gums receding and eventually teeth becoming loose.
If left untreated chronic periodontitis can lead to significant tooth loss as it breaks down the support structures like the periodontal ligament. The progression can be subtle with sufferers feeling no pain or minimal pain at first. Early detection and action is key to management. Regular visits to the dentist and good oral hygiene is crucial to prevent severe consequences of this type of periodontal disease.
To prevent any further deterioration and overall oral health when you have chronic periodontitis, treatment from an oral surgeon or specialist in gum diseases is necessary. Scaling and root planing can control the damage – more invasive surgical procedures are available if needed – to manage this common but serious condition.
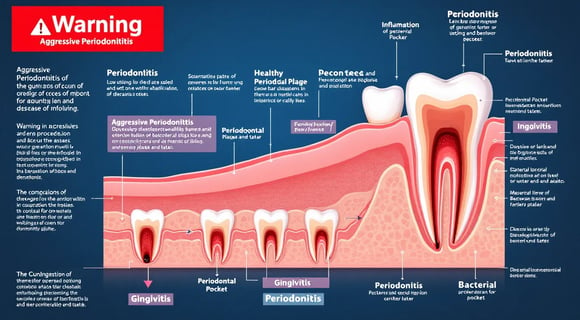
Aggressive Periodontitis: Rapid Onset
Aggressive periodontitis is a type of periodontal disease that causes rapid and severe destruction of the supporting structures of the teeth, affecting young people before they are 30 years old. This is different from chronic periodontitis as it can cause significant damage to the gums and bone with minimal plaque.
This virulent form usually starts around puberty, mainly affecting incisors and first molars with rapid loss of attachment. It is linked to certain pathogens like Aggregatibacter actinomycetemcomitans and has familial clustering which means genetic predisposition might be a factor.
The rapid progression of this aggressive form highlights the need to detect it early. Aggressive periodontitis without traditional risk factors like smoking requires close observation and potentially more frequent visits to the dentist to control it.
Necrotizing Periodontal Disease: Severe Infection
Necrotizing periodontal disease is a severe infection characterized by painful gum ulcers, severe inflammation and rapid tissue destruction. This condition presents with symptoms of severe gum pain, spontaneous bleeding, bad breath and loss of bone supporting the teeth.
Those with a history of HIV, malnutrition or significant stress are more prone to necrotizing periodontal disease. Diagnosis is based on clinical observation and microbiological tests that show a mix of microorganisms.
Treatment is necessary to manage. Common treatments are pain management, debridement of affected tissues and antibiotics for severe cases. Get professional help from an oral surgeon as soon as possible to prevent complications and maintain oral health.
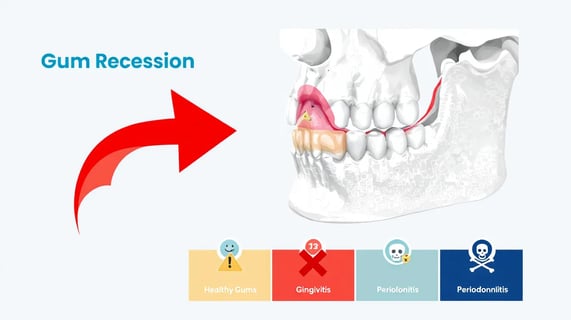
Gum Recession: Exposing Tooth Roots
The gums retracting from the teeth, also known as gum recession, exposes the tooth roots. This can be caused by harsh brushing, hormonal fluctuations, hereditary factors or periodontal diseases. The consequence of this gum tissue retraction is increased risk of sensitivity and decay.
To stop the deterioration caused by gum recession — a condition that cannot self heal — professional help is needed. Treatments like root planing, gum graft surgery and desensitizing products are used to stabilize receding gums and protect exposed roots from further damage.
Gum Abscess: Localized Infection
A gum abscess is a collection of pus caused by a bacterial infection confined to the tissue surrounding the gums which presents with discomfort, inflammation and a pocket of pus. Get this treated as soon as possible to stop the infection and maintain good oral hygiene.
The treatment for an abscess is to create an opening to drain it and then clean out the infectious material. Antibiotics may be given as a preventive measure against further infection and pain relievers available over the counter can help alleviate the pain. A dentist is best in managing gum abscesses.
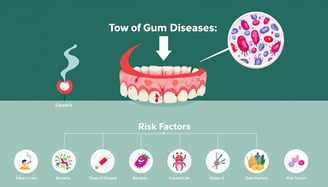
Risk Factors for Gum Diseases
Many risk factors contribute to periodontal diseases. The accumulation of bacteria below the gum line which is often due to poor oral hygiene can cause infection and swelling. Smoking worsens the progression of these diseases.
Even with good oral hygiene, genetic factors can predispose some to gum disease. As we age, the condition becomes more prevalent. It affects over 70% of people 65 years and above. Complicating this is a systemic condition like diabetes and blood disorders that makes one more prone to gum problems.
Symptoms of Gum Problems
Early detection of gum disease is key to preventing serious dental problems. Bad breath often indicates gum problems. If you notice bleeding during brushing or flossing, and red and swollen gums, these are usually the first signs of gum disease.
Other signs to look out for are tender gums and pus near where your teeth meet the gums. Changes in your bite or loose teeth can be signs of progressing gum condition which needs to be treated as soon as possible to prevent tooth loss and other oral health problems.
How Dentists Diagnose Gum Diseases
To diagnose gum diseases, dentists use various diagnostic methods. These include visual examination of the gums and teeth and periodontal probing with a small instrument to measure the gap between the gums and teeth. If the pocket depth is more than 3 mm it could be gum disease.
Dentists use X-rays to see if there’s bone loss around the teeth and to calculate clinical attachment loss to determine the extent of periodontal disease. Sometimes for a more precise diagnosis and detailed analysis of gum disease a tissue biopsy may be done.
Treatments for Gum Diseases
Treatment of periodontal disease usually starts with professional dental cleaning through scaling and root planing. Scaling removes tartar and bacteria from the teeth and below the gums and root planing smooths the root surfaces to prevent future tartar buildup.
Advanced treatment may involve flap surgery for better cleaning, bone grafting to replace lost bone and guided tissue regeneration for bone regrowth. Laser assisted procedures is a less invasive way of treating gum disease while preserving healthy tissue.
Gum grafting surgery is the most effective long term solution for gum recession. Dental bonding can cover exposed tooth roots, while treatments like fluoride varnish and desensitizing agents can alleviate sensitivity.
Home Remedies and Preventive Measures
While professional treatment is necessary, there are home remedies that can soothe sore gums and reduce inflammation. Rinsing with warm saltwater, hot or cold compresses and herbal pastes made from clove powder or turmeric can help. Homemade dental sprays with diluted essential oils and teabags high in tannins like black or green tea can also calm irritated gums.
A daily oral hygiene routine—brushing, flossing and regular dental check-ups is key to successful gum disease treatment and overall oral health.
Complications of Untreated Gum Diseases
If gum disease is left untreated it can lead to serious problems like bone and tooth loss. The progression of periodontal disease can exacerbate chronic conditions like cardiovascular disease, diabetes and neurological disorders.
Those with periodontal disease are more prone to severe cardiovascular events like heart attack and stroke. Gum problems can also increase the risk for oral cancer which is characterized by discolored spots or masses that last more than 2 weeks.
Prognosis and Management
The prognosis for periodontal disease can be wide ranging depending on how early it is detected and how soon treatment is done. If caught at the initial stage gingivitis it can be reversed with proper dental care and good oral hygiene. If it advances to more severe stages of periodontal disease damage may be permanent and the prognosis can be from fair to very poor.
Catching gum diseases early and acting fast is key to preventing complications. Regular visits to the dentist for check-ups and professional intervention is crucial in managing gum diseases by slowing down its progression and preventing further damage.
Although there is no cure for advanced periodontal disease once it’s established, management including professional treatment and strict oral hygiene can control the disease.
Can Gum Diseases be Prevented?
Good oral hygiene through twice daily brushing with fluoride toothpaste and flossing is key to healthy gums. These habits remove dental plaque which is the key to reducing gum inflammation.
Regular professional cleanings and dental check-ups is crucial to control the progression of gum disease. By following these preventive measures you can reduce your chances of getting advanced gum disease and overall oral health.
Smoking is a major risk factor for gum disease, as it weakens your immune system and makes it harder for your gums to heal.
Quitting smoking can significantly improve your oral and overall health.
Nutrients like Vitamin C, calcium, and Omega-3 fatty acids are essential for gum health and can help reduce inflammation.
Limit sugar intake, as sugary foods contribute to plaque and bacterial growth.
Conclusion
Knowing the types of gum diseases is key to good oral health. From reversible gingivitis to severe necrotizing periodontal disease each condition requires specific treatment and prevention. By recognizing the symptoms early and seeking professional care you can prevent the progression of the disease and complications.
Having a consistent oral hygiene routine, regular dental check-ups and knowing the risk factors can keep your gums healthy. Remember your oral health is part of your overall well-being and taking action now can save you from big problems later.
FAQs
What is the first stage of gum disease?
The first stage of gum disease is gingivitis which is inflammation of the gums and is reversible with proper care.
Act now and restore your gum health.
How can I prevent gum diseases?
Good oral hygiene is key to preventing gum diseases. Brush twice a day, floss regularly and visit the dentist for regular check-ups.
Follow these habits for overall tooth health.
What are the signs of chronic periodontitis?
Signs of chronic periodontitis are bad breath, receding gums, loose teeth and spaces between gums and teeth.
Address these signs immediately to prevent further oral problems.
How do dentists diagnose gum diseases?
Through a thorough examination which includes visual inspection, periodontal probes and X-ray for bone loss dentists can diagnose gum diseases to get an accurate oral health assessment.
What are the treatments for advanced gum disease?
For advanced gum disease scaling and root planing, flap surgery, bone grafting, guided tissue regeneration and laser assisted treatment are available.
Gum grafting can also treat gum recession.
Scaling and Root Planing: A deep-cleaning procedure where the dentist cleans below the gum line to remove bacteria, plaque, and tartar. They also smooth out rough spots on the root surfaces to help gums reattach to the teeth.
Antibiotics: Dentists may use antibiotics, in the form of topical gels, mouth rinses, or pills, to help reduce bacteria in the gums.
Flap Surgery: In this surgical procedure, the gums are lifted back to allow deeper cleaning of the roots, then stitched back in place to fit snugly around the teeth.
Gum Grafts: If the gums have receded significantly, a gum graft can cover the exposed roots. Tissue is usually taken from the roof of the mouth or a tissue bank and attached to areas where gums have receded.
Bone Grafts: In severe cases where bone loss has occurred around the teeth, a bone graft can be used to help regenerate lost bone.
Guided Tissue Regeneration: This technique helps regrow gum and bone tissue by placing a special material between the bone and gums to encourage growth.
Laser Therapy: Some dentists use lasers to remove infected tissue and bacteria from deep pockets in the gums, which can be less invasive and help reduce bleeding and discomfort.